Introduction
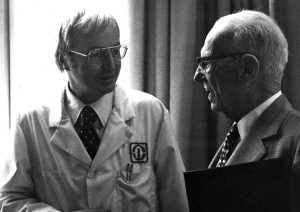
Polycystic Ovarian Syndrome (PCOS), also known as Stein–Leventhal syndrome is an enigmatic
and complex endocrine disorder originally described by Drs Irving Stein and Michael Leventhal in
1935. Their description of the disease remains the basis of its diagnosis to this day.
PCOS is the most common endocrine disorder in women of reproductive age, seen in as many
as 75% of anovulatory women. In a 2013 study, the condition was observed in 18.1% of Nigerian
women presenting in two infertility centres over a two-year period. Ultrasound findings suggestive
of PCOS are present in up to 20% of women, including those without symptoms. Specific criteria
must, therefore, be satisfied to establish a diagnosis of Polycystic Ovarian Syndrome.
Pathogenesis
The aetiology of PCOS is multifactorial, suggesting familial and genetic associations alongside a variety of environmental factors. The syndrome includes the presence of the following – elevated
Luteinizing Hormone (LH), insufficient Follicle Stimulating Hormone (FSH) and insulin resistance, all of which work synergistically to cause increased ovarian growth, ovulatory dysfunction and
excessive androgen production.
Obesity may increase the degree of insulin resistance and consequent hyperinsulinemia.
Elevated insulin levels cause a decrease in the synthesis of two important binding proteins, namely – insulin-like growth factor binding protein (IGFBP-I) and sex hormone binding globulin (SHBG) which in turn leads to an increase in the level of androgens present in the circulation. Many of the clinical manifestations of the syndrome arise from hyperinsulinaemia and hyperandrogenemia.
Diagnostic criteria

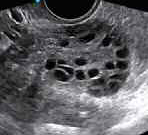
Figure 1: Transvaginal ultrasound images of polycystic ovary (left) & normal ovary (right)
The rotterdam conference held in 2003 attempted to standardise the diagnostic criteria for PCOS
and reached a consensus on the existence of 2 or more of the following features:
1. Oligo-ovulation or anovulation
2. Clinical and/or biochemical signs of hyperandrogenism (HA)
3. Polycystic ovarian morphology (PCOM) – i.e. 12 or more follicles measuring ~2-9mm in diameter or ovarian volume of >10cm3 on transvaginal ultrasound scan. A single ovary may fulfil the sonographic criteria. All other causes of excessive androgenic secretion, such as congenital adrenal hyperplasia (CAH), Cushing’s syndrome, androgen-secreting tumours must have been excluded.
Serial #: K600-5348
Width: 3060
Height: 2036
Date: 06/25/2001
Time: 16:35:27
DCS4XX Image
FW Ver: 051998
TIFF Image
Look: Portrait
———————-
Counter: [14]
ISO: 80
Aperture: F18
Shutter: 200
Exposure: M
Exp Comp: 0.0
Meter area: Part
Flash sync: None
Flash comp: 0.0
Drive mode: Sing
Focus mode: One
Lens (mm): 0039
Clinical features
The clinical manifestations of PCOS may include a range of menstrual abnormalities,infertility, skin manifestations, hirsutism and systemic metabolic disorders. Common menstrual abnormalities may
CASE SCENARIO
A 30-year-old woman presents with a background history of menstrual irregularities and more recent (2-month) delay in her menstrual cycle.She has battled with acne and facial hair for most of her adolescence and adult life and regularly shaves under her chin and abdomen (at least
once a month). She has tried unsuccessfully to conceive for the last 18 months. Her BMI is 30.5 and she has a waist circumference of 95cm.Her doctor suspects a diagnosis of Polycystic Ovarian Syndrome (PCOS).
include irregular, delayed or absent menstrual periods, breakthrough bleeding or persistent heavy bleeding. Patients may also present with features of excessive androgen secretion such as acne, oily skin, hirsutism (male pattern of hair distribution), alopecia and (rarely) clitoromegaly.
Many patients diagnosed with PCOS may have a high body mass index (BMI) although 25-50% of these women may also have a normal BMI with or without truncal obesity.
Infertility observed in these women may arise from anovulation,infrequent ovulation, hyperandrogenism or deranged LH / FSH secretion.This form of infertility often responds to induction of ovulation.
Acanthosis nigricans is a skin manifestation characterised by a dark,velvety appearance typically affecting the axilla (armpit), nape (back of the neck), area underneath the breast and skin flexures elsewhere in the body. Acanthosis nigricans is seen in 5% of PCOS patients and is typical of the existence of insulin resistance.
In pregnancy, PCOS may also present with gestational diabetes,pregnancy-induced hypertension, pre-eclampsia, preterm and caesarean delivery, recurrent miscarriage, neonatal hypoglycaemia and perinatal death.
Complications
The long-term consequences of PCOS are usually established by 40 years of age and consistent
with a pattern of hyperinsulinaemia arising from insulin resistance.
30 to 40% of women with PCOS develop glucose intolerance while 10% may go on to develop
type 2 diabetes mellitus (T2DM). The risk of developing type 2 diabetes is higher in obese women
but is also present in lean patients with a diagnosis of PCOS.
The combination of hyperinsulinaemia, hyperandrogenism and obesity, all known risk factors
for cardiovascular disease, predisposes the patient towards atherosclerosis, hypertension and
myocardial infarction. Patients are additionally predisposed to endometrial hyperplasia and (possibly)endometrial cancer due to the unopposed effect of oestrogen on the endometrium; hence
the importance of conducting a full evaluation of all cases of abnormally heavy or prolonged
vaginal bleeding.
Patients with PCOS are also at risk of obstructive sleep apnoea and psychiatric disorders such
as depression, anxiety, binge-eating and bipolar disorder. All of these features may be directly
related to the symptoms and complications of PCOS (obesity, infertility, hirsutism, miscarriage) or indirectly linked with the patient’s awareness of the potential complications of the disease.
Management
The management of PCOS is guided by its symptoms. The general principles of treatment are
as follows:
1. restoration of menstruation, ovulation / ovulatory cycles and fertility
2. Treatment of acne and hirsutism (features of excessive androgen production)
3. Prevention of long-term complications (as outlined above)
Investigation
- Pregnancy tests (using beta HCG)
- Hormone profile – FSH/LH, Prolactin, TSH, mid-luteal phase progesterone and Androgens(including testosterone and dihydroepiandrosteindione sulphate)
- Imaging – Transvaginal ultrasound scan to assess the ovaries and endometrial thickness
- Sex hormone binding globulin (SHBG) and the total testosterone to estimate the free androgen index, testosterone /SHBG X 100
- Further investigations to exclude other causes of androgen excess (CAH, Cushing’s syndrome,androgen-secreting tumours) – 24-hour urinary free cortisol, 17 hydroxyprogesterone
- Tests for infertility – Seminal fluid analysis (SFA), hysterosalpingography (HSG) and laparoscopy (if necessary)
- Additional tests to screen for long-term sequelae – Oral Glucose tolerance test (OGTT),lipid profile, endometrial biopsy
Treatment principles
- Dependent on symptoms as well as patient’s desire
- Options – conservative, pharmacological or surgical
Weight loss reduces insulin and androgen levels – a 10% loss in weight can restore ovulation
and regular periods. Exercise, diet and lifestyle modification are therefore effective methods of
conservative treatment.
Menstrual irregularities may be treated with the combined oral contraceptive (COC) pill (as first line) or Medroxyprogesterone acetate / Norethisterone for 12 days every three months for cases in which the COC pill is contraindicated. The COC pill may be used to treat acne and hirsutism in PCOS patients while offering (simultaneous) protection against endometrial hyperplasia.
Hirsutism may be treated physically by shaving, chemical depilation/bleaching, waxing, plucking,electrolysis and laser therapy. Pharmacotherapy will typically comprise treatment which combines the use of oestrogen with a non-androgenic progestogen such as desogestrel or norgestimate.Dianette is an effective combined oral contraceptive pill which includes a combination of ethinylestradiol (30mcg) and a potent anti-androgen progestogen (cyproterone acetate – 2mg).
Other forms of treatment for hirsutism include spironolactone, finasteride, flutamide and
eflorthinine topical cream.
Ovulation induction
These forms of treatment are directed towards ovulation induction and restoration of
ovulatory cycles.
Clomiphene Citrate (CC) – a selective oestrogen receptor modulator, is administered at a dose
of 50-150mg daily for five days starting on day 2 of the menstrual cycle. Ovulation is achieved in
75% of cases, and 35-40% of these patients are expected to achieve pregnancy. Side effects
include hot flushes, bloating, abdominal distension, abdominal pain from enlarged ovaries, multiple pregnancies and ovarian hyperstimulation syndrome.
Letrozole – an aromatase inhibitor is more effective than Clomiphene alone. It is administered at 2.5-7.5mg daily in a similar regimen to Clomiphene Citrate.
Side effects include sweating, bone pain, hot flushes, back pain and nausea. Letrozole carries
a lower risk of multiple pregnancies.
Other drugs potentially useful for this purpose include tamoxifen and gonadotrophin injections.
Laparoscopic ovarian drilling using diathermy is effective in triggering ovulation in women with PCOS– 4 points are drilled to a 4mm depth with 40 watts and for 4 seconds in each ovary. The procedure has replaced the more traditional wedge resection of the ovaries pioneered by Stein and Leventhal in the 1930s. In Vitro Fertilization remains a viable option for management if all intervention fails.
Metformin – administered in doses of 1500-2000mg daily in divided doses can be used in
women who are clomiphene resistant. It is associated with a higher rate of pregnancy but no
difference in live birth rate. Metformin is useful in cases of co-existent glucose intolerance, T2DM and possibly more effective in obese women.
Metformin encourages fertility and controls (PCOS) symptoms by increasing insulin sensitivity in
patients with PCOS. Side effects include nausea, vomiting, abdominal discomfort, diarrhoea and
loss of appetite.
read more
Disclosure forms provided by the author are available at NEJM.org.
Editor’s note:
Author Affiliations
Prof. Bosede B Afolabi MBChB (Ife), DM(Notts), FrCOG, FWACS, FMCOG Professor of Obstetrics and Gynaecology College of Medicine, University of Lagos.
Supplementary Material
| Disclosure Forms | 83KB |
Add your Comment
Add your Comment
Leave a Reply
You must be logged in to post a comment.
BHQJ 2018 ; 001:34-36
Related Article 
Medical Negligence & the Law5th May 2018 . Atrogenic harm is a matter of significant concern in Nigeria admin
Colorectal Cancer Overview5th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] Introduction Colorectal cancer is a major admin
Funding Healthcare Services in Nigeria – A conundrum of demand, policy and supply!5th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] Doctor, I happy say na you admin
5 “Provocations” of Healthcare Quality Reform6th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] n the four decades since he admin
Health Insurance, Activism & Urgent Change6th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] AR: Dr Soyinka, it’s wonderful to admin
Anne Olowu talks about her “Masterclass” experience6th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] As I suspect is the case admin
Stomach & Oesophageal Cancer in Nigeria6th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] Gastric and Oesophageal (Upper GI) cancers admin
Setting out the Stall!7th May 2018 . [dkpdf-columns columns="3" equal-columns="false" gap="10"] "The drawbacks of our false knowledge admin




Leave a Reply
You must be logged in to post a comment.